What to Eat on an Ulcerative Colitis Diet and What to Avoid Eating.
Ulcerative Colitis Disease is a chronic inflammation of the digestive tract. The large intestine and the rectum are affected in Colitis. Inflammation affects the innermost lining of the colon. Colitis is found in large, continuous sections. The inflammation causes abdominal pain, cramping, and diarrhea. Living with this pain and GI distress can cause fatigue. You may lose weight or struggle to maintain a healthy weight.
Table of Contents
How does your life work when your stomach is tied up in knots? If you have Ulcerative Colitis Disease, you may feel your life has been interrupted. How do you get back into the game? What can you eat on an Ulcerative Colitis Diet?
The cause of Ulcerative Colitis Disease is unknown. If someone in your family has Ulcerative Colitis, you may be more at risk. Researchers are studying the role of genes and the body’s immune systems. There are also studies on environmental factors such as smoking. Depression, sleep disturbance and stress are factors that may also increase the risk of Ulcerative Colitis Disease. Ulcerative Colitis is a type of Inflammatory Bowel Disease (IBD) but follows a different nutrition plan from the similar crohn’s dietary restrictions.
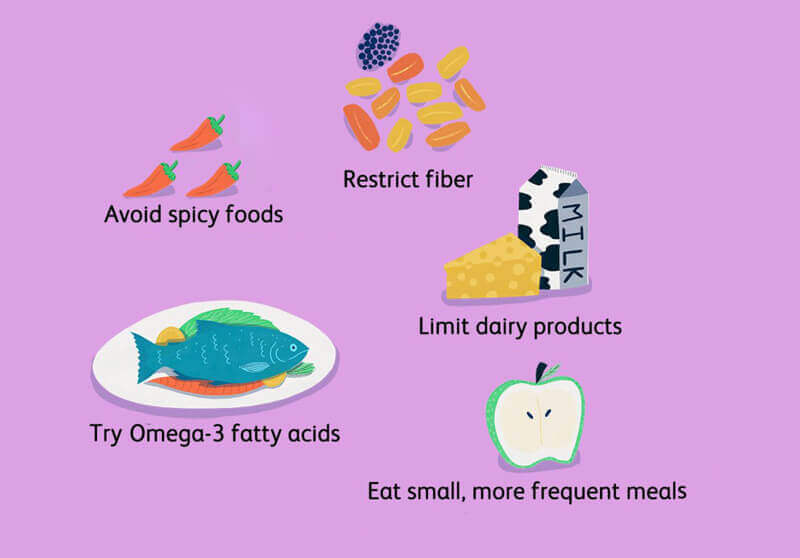
What you eat on an Ulcerative Colitis diet foods can cause symptoms to be triggered. The resulting inflammation can prevent your body from absorbing the nutrients in those foods. Poor nutrition is common during flare ups. To eat properly on Ulcerative Colitis Disease and help manage symptoms, pick foods that are nutrient-rich and minimally processed. Focus on healthy food to fuel your body and help your gut heal.
Ulcerative Colitis Diet Foods to Avoid
So, what can’t you eat on an Ulcerative Colitis diet? Certain Ulcerative Colitis foods to avoid may help reduce the severity of your symptoms. However, the Ulcerative Colitis foods to avoid vary for individuals. One key to managing flares is to learn your individual trigger foods. A registered dietitian nutritionist (RDN) can help you design an eating plan based on your unique needs.
Although the Ulcerative Colitis Diet is not set in stone taking these 3 steps can help you manage your symptoms:
Avoid food high in saturated fat. Marbled meats, whole milk, sausage, and butter contain high amounts of saturated fat. Research has found that high intakes of saturated fat may lead to inflammation in the body. Avoiding these foods may help reduce symptoms. Not symptomatic, reducing your saturated fat is heart-healthy!
Restrict highly processed foods. Added sugars, saturated fats, salt, and preservatives are often added to these foods. Plus, these items often have sugar alcohols which can make diarrhea worse. Examples of sugar alcohols are mannitol, sorbitol, and xylitol. They are common in sugar-free drinks, gum, and candy. Sugar-free gummy vitamins may also contain sugar alcohols.
Alcohol. Be it beer, wine, hard cider, or the hard stuff, restricting alcohol can help control your flare-ups. The reason is that these drinks can interfere with your prescribed and over-the-counter medicines. Thus, if you drink alcohol, you increase your risk of relapse.
What to Eat? Ulcerative Colitis Foods During a Flare:
Selective Ulcerative Colitis foods during a flare is something that needs to be approached with caution – especially initially. When you are in pain, feeling bloated, and just don’t feel like eating, choose foods that are easy to digest.
Select refined grains. Refined grains are easier to digest than whole grains. So, select white bread, white rice, and white pasta. Yes, a dietitian is recommending you eat white grains! These foods are sources of B vitamins and Iron.
Choose low fiber vegetables and fruits. Low-fiber vegetables are well cooked or canned veggies, mashed potatoes without the skins, and string beans. Cooking veggies helps to break down the fiber. So, when you are flaring, avoid salads and other dishes with raw vegetables. Also, remove the skin from raw veggies and fruits and avoid produce that has seeds such as strawberries and raspberries. Low-fiber fruits are bananas or cantaloupes. For a nutrient-rich drink, reach for low-sodium vegetable juice.
Use unsaturated fats. Cook with small amounts of heart-healthy unsaturated oils. Try different oils (olive, avocado, canola) to replace butter or stick margarine. Aim for a fat intake below 35% of your daily calorie intake. A low-fat diet may help to prevent bloating, cramping, and diarrhea.
Reach for calcium-rich foods. For example, low-fat dairy products (lactose-free if needed), canned salmon, and soy products. Oat, soy, or rice drinks enriched with calcium are another option.
What to Eat? Ulcerative Colitis Diet Foods During Remission:
What you should eat on an Ulcerative Colitis diet plan is very individual but let’s get acquainted with what it takes to be on an Ulcerative Colitis diet plan when your disease is not active:

What You Can Eat on an Ulcerative Colitis Diet.
Eat a variety of vegetables and fruits.
Select the refined grains. These have been milled to remove the bran and germ, (the in- soluble fiber in the bran and germ) may increase symptoms.
Include protein-rich foods.
Get enough calcium.
Drink plenty of fluids.
Your Ulcerative Colitis diet plan can even be more liberal when your symptoms subside but remember to:
Go Slowly. Gradually add more foods back into your diet. Shift to whole grains and those colorful veggies and fruits. Start with small amounts of these foods. If your symptoms act up, add that item to your potential list of trigger foods. You can try eating that food at a later time.
Eat 5 or 6 small meals per day. Go easy on your GI tract. Large meals can flare your symptoms and make you feel bloated.
Stay well hydrated. Sip on water throughout the day. As you add back in fiber, getting enough to drink is important. Fiber without adequate fluid intake can lead to constipation.
Avoid your trigger foods. Focus on the foods you can eat and enjoy. Create a list of substitutions for your trigger foods.
Practical Advice for What to Eat on an Ulcerative Colitis Diet
Many organizations post food shopping lists for Ulcerative Colitis Disease. These resources are a good starting point. Download a list and make it your own. Mark off your trigger food and add foods that you can safely eat.
Plan ahead and enhance your weekly menus with MealPro Ulcerative Colitis meal delivery service. These anti-inflammatory meals are designed to eliminate known trigger foods and reduce flares.
Roasted salmon: This meal is full of flavor while providing healthy omega-3s with a portion of asparagus and yellow bell peppers. Roasted potatoes round out the meal for a satisfying choice in carbs.
Turmeric Turkey: Lean turkey seasoned with the anti-inflammatory spice turmeric. Served with fresh green beans and bake yams. Rice is the foundation of this meal.
So, can Ulcerative Colitis symptoms change the way you eat? Yes. Although it is possible to adjust the foods you eat to improve and enhance your quality of life.